.:: What is prolapse?
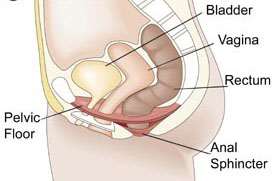
Pelvic organ prolapse is a relaxation of pelvic structures, which may lead to extreme discomfort and a protrusion of tissue from the vaginal opening. it is very similar to hernias. They are both due to weakness of the supporting tissues. Genital prolapse is due to weakness of the pelvic floor which is composed of muscles, collagen, connective tissue and fascia that extend from the pubic bone anteriorly to the sacrum posteriorly. Problems with sexual activity, as well as bowel and bladder dysfunction, may occur. Prolapse can occur quickly, but usually happens over the course of many years. There are various types of prolapse, which can occur individually or together. More informations are found by clicking on the GLOSSARY OF TERMS section and FAQ.
.:: Types of prolapse:
* Cystocele
Cystocele
Is experienced as a bulge in the vagina from the top, which comes right down to the vaginal entrance and even through the entrance. Cystoceles are commonly accompanied by urinary incontinence due to a bladder neck support deficiency. However not all patients with cystoceles are incontinent. Some very large cystoceles can actually obstruct the flow of urine and cause backpressure on the kidneys. Cystoceles can also mask incontinence which becomes obvious once the cystocele is reduced. Cystoceles can occur due to a central stretch in the support (central defect) or can be due to the supporting structure tearing away from the pelvic wall (paravaginal defect).
* Uterine Prolapse
Uterine Prolapse
The uterus slides down from its normal position and descends to or outside the vaginal opening. When the entire uterus lies outside the vaginal opening it is called as procidentia. The weight of the uterus and the blood vessels which are dependent cause the organ to become swollen and easily susceptible to infection. Ulcers are very common in uteri which prolapse. Moreover difficulty in sexual intercourse may also result. When the uterus comes down it can pull the urethra along with it resulting inurinary incontinence. Sometimes the prolapse might be so massive that it can actually mask the incontinence. Hence women who have surgery for prolapsed uterus comeback within a short period of time with incontinence problems.
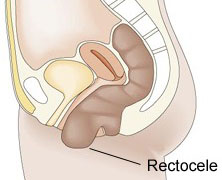
* Rectocele
Rectocele
Rectocele is the bulging of the bowel into the vagina. This occurs because the supportive layer of the vagina has torn away or due to muscle injury. Women with rectoceles have a problem emptying their bowel. They develop something known as obstructed daefecation where they are not able to pass motion in-spite of repeated straining. Hence these women have to digitate (to push with their fingers inside the vagina inorder to empty their bowel). Repeated straining like this can also cause the perineal area to sag down.
* Vault Prolapse
Vault Prolapse
This occurs in women who have their uterus removed. The top of the vagina known as the vault comes down. This can either be partial or total where it comes fully down. Women might experience trouble with emptying their bladder or might have difficulty during intercourse. The commonest reason for this occurring is that the uterine supports that were cut during the hysterecytomy were not reattached to the vault.
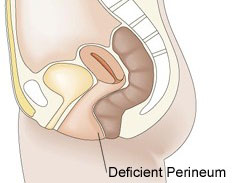
* Deficient Perinium
Deficient Perinium
Lack of support of the perineum ( the area between the entrance of the vagina and anus ) causes a deficiency rather than a prolapse.
.:: How common is prolapse?
50% of women who have had children complain of some vaginal prolapse but only 10 to 20% of these women seek medical attention. Over 10% of women undergo pelvic floor surgery for the management of Pelvic organ prolapse and or Urinary incontinence. Up to 1/3 of these women will undergo repeat surgery. The incidence of surgery for prolapse seems to increase with age. The peak age group for women undergoing urinary incontinence surgery is the 40-50 year old group. Increasingly we are seeing younger women who are unwilling to “put up with” these problems.
.:: Causes of prolapse:
The causes of any prolapse is multifactorial. Simply, the supporting tissue is unable to cope with the strains being placed upon them. In the case of genital or vaginal prolapse these causes can be divided into two groups. Factors that cause increased abdominal pressure are at risk of causing the pelvic floor to fail or be damaged.
These commonly include:
- Obesity
• Chronic chest problems causing chronic coughing
• Constipation or straining to defecate
• Work or lifestyle that requires heavy lifting or abdominal straining.
• Pregnancy
• Childbirth:
• Pelvic masses like uterine fibroids or ovarian masses; rare but can occur.
The second common cause is a pelvic floor that is weak or damaged and is unable to effectively resist normal increases in abdominal pressure.
Common causes of pelvic floor weakness include:
Neuropathy: the nerves supplying the muscles are damaged. Common causes of neuropathy to the pelvic floor include age and childbirth.
• Inherited weakness of pelvic floor collagen, fascia or muscle.
• Postmenopausal women are at increased risk.
• Estrogen deficiency may be a risk factor.
• After some Gynecological operations: For example posterior uterine wall prolapse is common after colposuspension. Deficient perineum is common after vaginal birth and episiotomy repair.
.:: What problems does prolapse cause?
Many women with mild to moderate prolapse are unaware of the problem. Most symptoms of prolapse are generalizable to all sorts of prolapse and usually deteriorate as the day progresses and after long standing and improve with lying down.
These symptoms include:
- Bulge, heaviness or dragging sensation.
• Backache.
• Vaginal irritation or dryness or even sometimes ulcers.
• Need to push the vagina back especially after straining (defecation).
• Sexual Intercourse impossible or embarrassing.
• Chronic pain in the region of the pelvis.
• Decrease in sexual satisfaction.
Bladder symptoms that can be associated with prolapse include:
- Urinary frequency and urgency.
• Stress urinary incontinence.
• Voiding difficulties.
• Inability to pass urine without reducing the prolapse back into the vagina.
• Rarely the upper renal tracts can be obstructed due to kinking of the ureters that drain kidneys to bladder.
Vaginal prolapse can also cause bowel symptoms including:
- Incomplete bowel emptying.
• Obstruction at defecation due to faeces lodging in the rectocele.
• Constipation may be caused by the rectocele.
• The need to reduce prolapse (Insert finger in the vagina) to empty the bowel.
• If the rectum prolapses out of the vagina fecal incontinence may occur.
©2018-2023, All rights reserved to Arab Center for Urogynecology and Infertility. Powered By Creativity Design Studio |جميع الحقوق محفوظه للمركز العربي للجراحة البوليه النسائية و العقم | الدكتور رامي محافظة